Sinus lift procedure
Interactively coordinate synergistic solutions via user friendly sources. Completely reconceptualize maintainable services before inexpensive action items. Enthusiastically e-enable dynamic functionalities rather than fully researched outsourcing.
The first phase of the dental implantation procedure
Average implantologist makes the most mistakes before starting a dental implant placement. If an implantologist skips any of the steps of the first phase of the dental implantation procedure (presurgical) or make wrong decisions, he predefines the complications at the end.
The dental implantation procedure is 20% about skills and 80% about knowledge.
— Dr. Anton Gerasimov
The first talk about the dental implantation procedure
During the first talk, an implantologist can evaluate the clinical situation and outline the approximate steps involved in the treatment. To ensure greater accuracy, the patient should provide all relevant medical data, X-rays, and CBCTs (Cone-beam computed tomography) in advance.
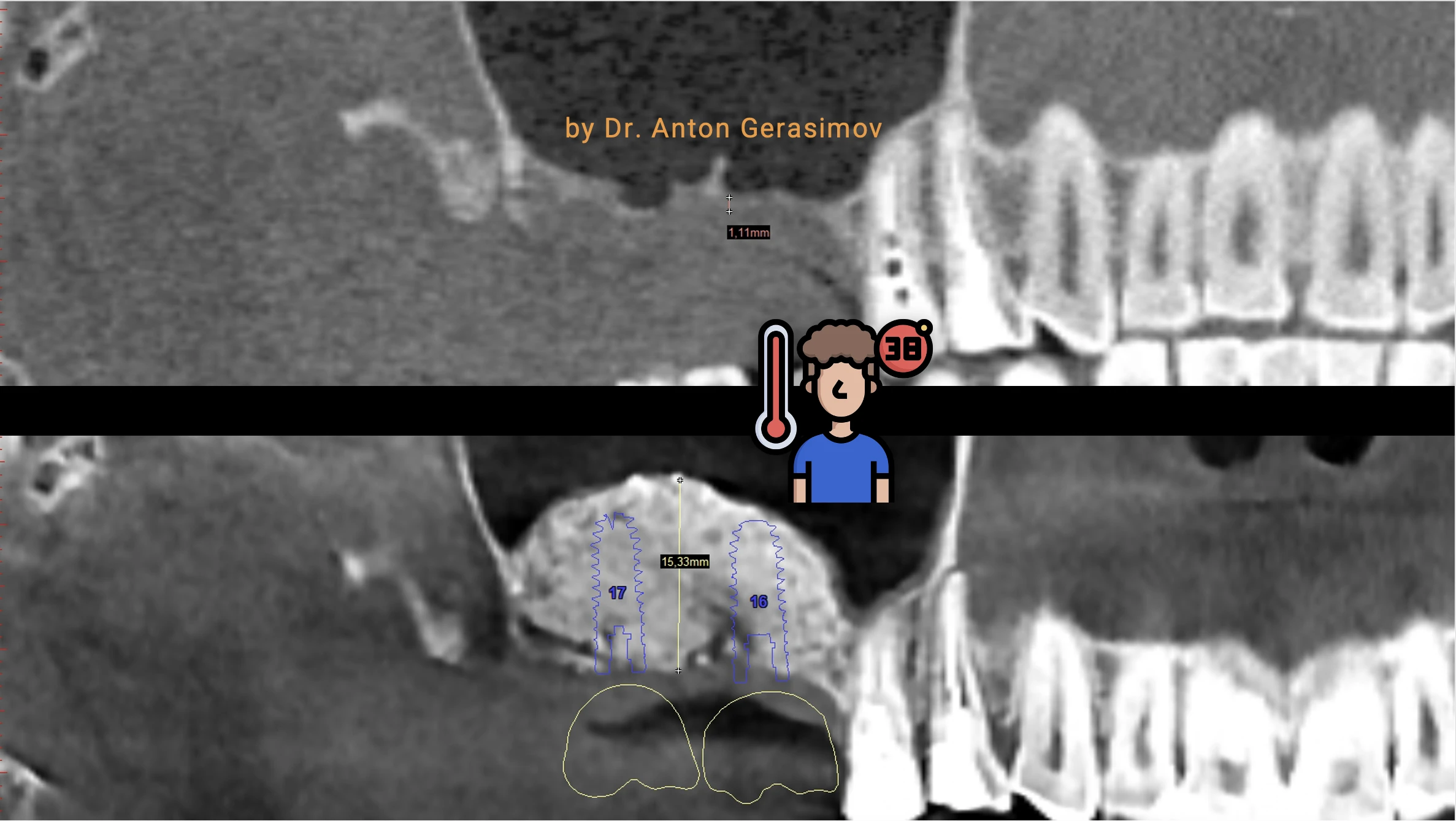
CBCT of jaws for the pre-assessment of the current situation
Actual CBCT must be evaluated before developing the treatment plan. “Actual means that it should be not older than one year, and no surgeries on jaws should be done after it and two months before it. If no such CBCT is available at that moment, then it’s time to do it.
EXAMINATION OF THE ORAL CAVITY By the implantologist
The fundamental factors for the implantologist here are the range of mouth opening and gag reflex. The former can sometimes affect the length and position of dental implants, while the latter can influence the type of anesthesia used. In addition, if a dental implant is planned for the esthetic zone, the smile line must be defined. Finally, an examination will help to clarify the diagnosis of diseases revealed on the CBCT.
Facultative consultation with General Health Doctors and other colleagues, all the diagnostics needed
This step should not be overlooked or underestimated. A profound general health check is part of the nonmaleficence and safety principle. An implantologist will reveal all comorbidities and refer to colleagues for a consultation to integrate the dental implantation into the comprehensive treatment plan. This step could be started as soon as the patient fills out the medical questionnaire.
Implantologist consultation with comprehensive treatment plan presentation
If the consultation was started without previous steps, there is a possibility that a treatment plan would be subject to change in the future. While this possibility cannot be eliminated entirely, appropriate preparation and the doctor’s deep knowledge of his and related specialties will clarify to the patient all the details of the whole treatment at this step already. It is always better to follow through with a plan than to wait and react to circumstances.
Informed consent for the dental implantation procedure, all questions to be answered
It is a time for a patient to make a decision. Does the offered treatment plan appropriate according to time and expenses, or an alternative way of treatment would be chosen? Are there any questions to answer? Do not be shy to ask at this step. If a patient changes their mind after this step, the process and results could be far from optimal.
Facultative provisional prosthetics for the whole period of treatment
If the treatment plan will take months and a patient needs teeth just “yesterday,” provisional prosthetics could be the answer. However, dentures are not recommended as a temporary measure for dental implantation procedures as they can accelerate bone resorption and contribute to gum recession.
Facultative general health stabilization
Many general health diseases influence dental implantation success. While very few are absolute contraindications, most must be stabilized in advance. Therefore, an oral surgeon should be in contact with general health doctors during and after this step.
Sanitation of the oral cavity before the dental implantation procedure
Caries, old fillings, crowns, and impacted wisdom teeth can be the source of infection during the dental implantation procedure. Moreover, proper sanitation of the oral cavity is essential not only for successful dental implants but also for the health of internal organs and systems such as the cardiovascular and endocrine systems.
Facultative periodontics treatment
If generalized periodontitis is diagnosed, it is essential to incorporate periodontal treatment into the plan. Failure to do so will lead to inevitable periimplantitis shortly after dental implant placement. Additionally, untreated periodontitis raises the risk of atherosclerosis and its associated complications.
Facultative orthodontic treatment
Occlusion refers to how the teeth come together and function during chewing. Improper occlusion can cause damage to teeth, crowns, bridges, veneers, and even all components of dental implants. Fortunately, orthodontic treatment can be done concurrently with dental implant procedures to ensure proper alignment and function of the teeth.
Tooth extraction (read carefully)
Nobody will extract a tooth without reason. The most frequent causes of teeth extraction are related to an infectious process in the tooth or periodontium. Therefore, freshly extracted sockets will contain some infection in most clinical cases. Antiseptic usage does not guarantee the killing of 100% of infection. At the same time, “antiseptic mouthwashes inhibit cell viability and alter the morphology of osteoblastic precursor cells irrespective of brands, treatment time, or alcohol content” (In-Seok Song et al., 2019). So antiseptics inhibit osseointegration of the dental implant if used directly on the bone. For this reason, it is more predictable to place a dental implant, NOT AT THE SAME time as the tooth extraction.
It must be a grave reason or a simple lack of knowledge to go against biology
— Dr. Anton Gerasimov
Facultative provisional prosthetics for the extracted tooth
With a patient’s request, one of the following provisional prostheses can be created:
- Essix retainer with a tooth
- Maryland bridge
- Provisional bridge
- Composite provisional tooth
Eight weeks for wound healing and regeneration (read carefully)
What I recommend
Early dental implantation (up to 8 weeks after tooth extraction) is the protocol I have been offering to my patients for almost 20 years. By means of observation of thousands of dental implant cases, I found this protocol to be optimal.
It has a number of benefits:
- Guaranteed wound healing of infection, as it’s enough time for the body to clean the extraction socket
- Soft tissues are able to regenerate completely, providing a stable and healthy environment for the dental implant
- An implantologist doesn’t have to divine how the regeneration will go in the exact case. He sees it
- Processes of bone regeneration are at the active phase
- The final result is higher because of the best bone preservation
- It is easier to perform so that the patient will suffer less
- It is cheaper for a patient: early implantation can often eliminate the need for additional procedures such as bone or soft tissue grafting, usage of membranes, and grafts
And some disadvantages:
- A dental implant must be placed in the first eight weeks (Everything depends on the patient)
- The temporary tooth must not be fixed on the implant. Other types of fixation are preferable. (Easy to manage)
- Manufacturers of dental materials earn less (I do not care)
- Doctor’s fees are less (I do not care)
- The patient may leave and choose another implantologist (I do not care)
Mythbreaking
If you heard an opinion that immediate dental implantation (dental implant on the same day of tooth extraction) helps to keep your bone, they are wrong. Remember that an opinion is the lowest proof ever. The strongest evidence in medical science is a systematic review and meta-analysis. And here it is the systematic review and meta-analysis, which says that “data of changes in peri-implant marginal bone level demonstrated significantly less marginal bone loss for implants placed using the early placement protocol (8 weeks after tooth extraction) compared with those placed in fresh extraction sockets (immediate or same day implantation) (Seyed Hossein Bassir et al. 2019)”.
Immediate implant placement (on the same day of tooth extraction) is "good" because it's so easy to offer, and the patient won't go anywhere from you, so it's not about medicine
— Dr. Anton Gerasimov
CBCT of jaws to check wound healing and regeneration process
This step finally reveals how the healing and the regenerative processes will go in the exact clinical case. And this CBCT’s original DICOM files are used in professional 3d modeling software to start a project. Afterward, the implantologist will use this project to plan dental implantation, sinus lift, or bone grafting.
Facultative bone transplantation or sinus lift
Please refer to relevant articles to study further.
A sinus lift may be indicated in the region of the molars and premolars (teeth numbers 7, 6, 5, 4) and very rare in the area of a canine and lateral incisor (teeth numbers 3 and 2) of the upper jaw. On the other hand, bone grafting procedures may be indicated in any region of both jaws with insufficient bone volume for implant placement.
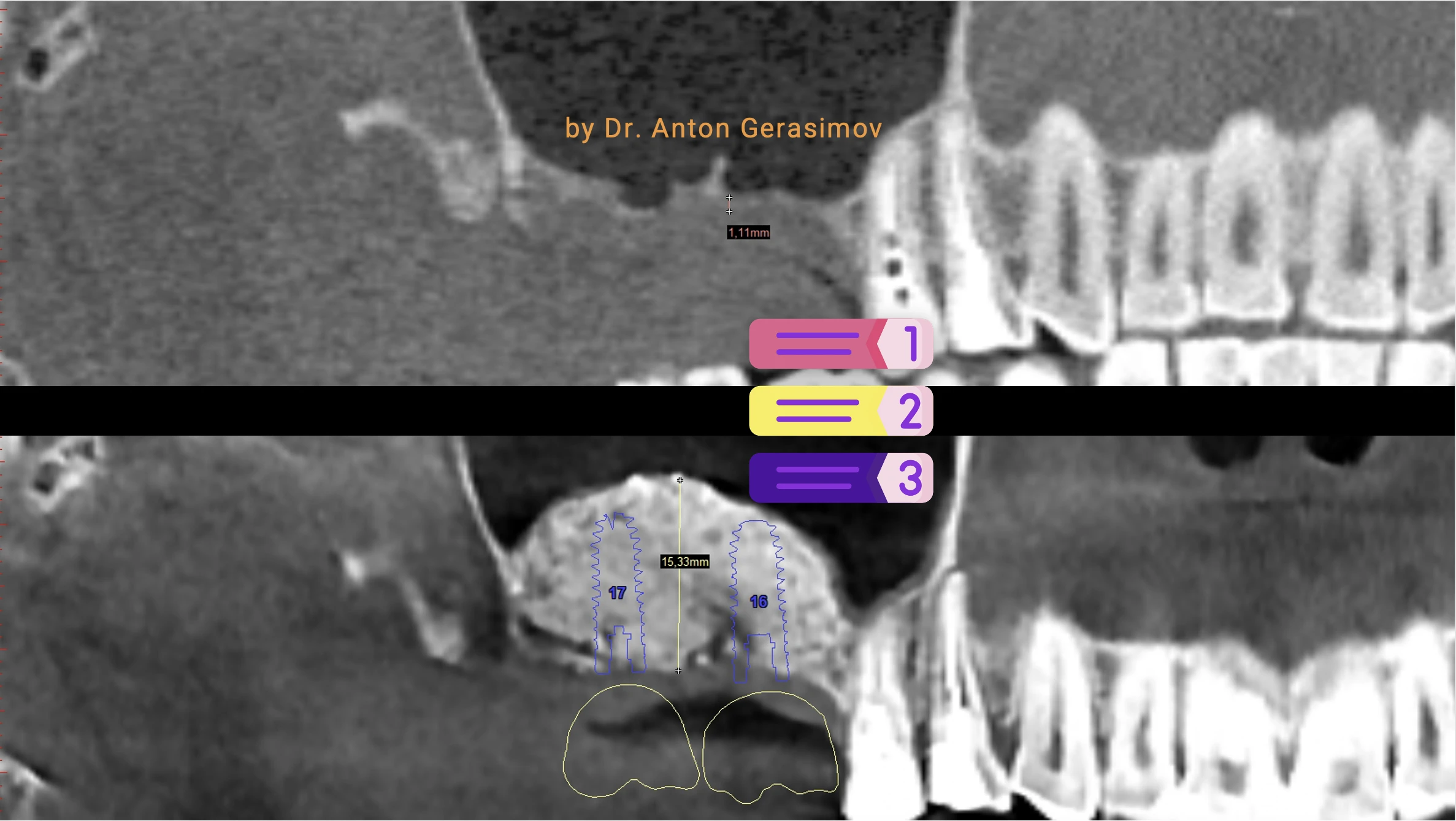
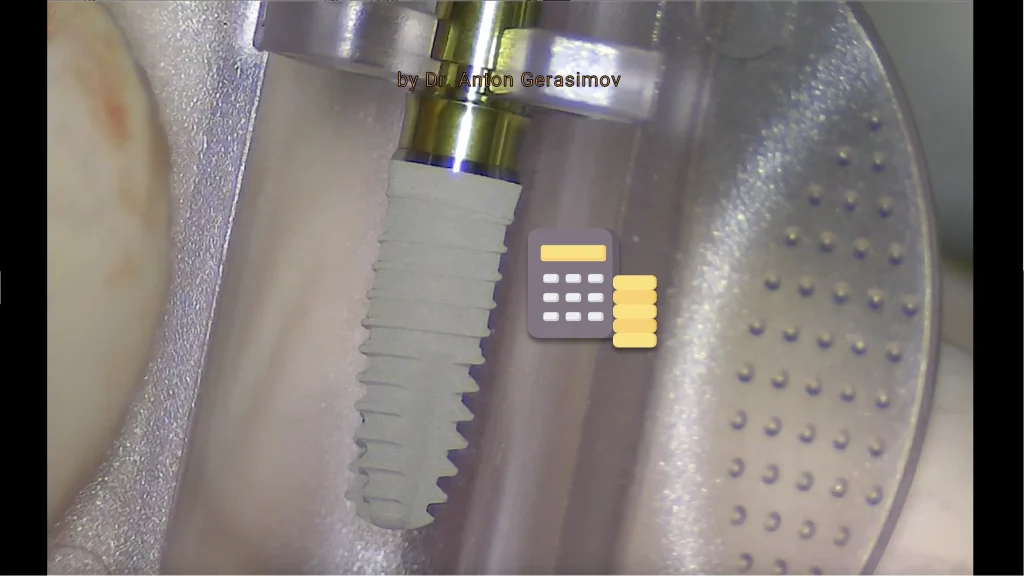
Pre-planning of the dental implantation procedure with computer-assisted design software, choice of the best dental implant for the clinical situation, surgical guide fabrication
It’s not something new. I’ve been performing computer-assisted modeling of every single dental implantation since 2004. The best dental implant for the patient must be chosen precisely. Despite the fact that the best dental implant does not exist, there is the correct size of the dental implant, which an implantologist will define with the computer-assisted design.
Then the computer plan is used during the actual surgery. In some clinical cases, the surgical guide is indicated. Why not always? Because if the surgical guide does not add a tangible improvement compared to routine measurements, an implantologist should know that a surgical guide could potentially increase the risks. For example, there is still controversy about whether “preparing an implant site with using surgical drill guides generates heat more than classical implant site preparation regardless of the irrigation type.” (Ferhat Misir et al. 2009). And the heat could be the reason for periimplantitis or implant failure.
Professional oral cavity hygiene
The dentist or dental hygienist will thoroughly clean, including scaling and root planing, to remove any plaque or tartar buildup that can lead to gum disease. They may also use an ultrasonic scaler or air polisher to remove surface stains and polish the teeth. In summary, professional oral cavity hygiene is a crucial step in preparing a patient for dental implantation to minimize the risk of infection.
THE SECOND PHASE OF THE DENTAL IMPLANTATION PROCEDURE
I’m doing a dental implant placement in 12 to 15 minutes. At the same time, all the previous steps can take from hours to months. Can we skip everything above? Sometimes we can skip facultative steps. But meticulous, “lege artis” preparation increases safety, and predictability decreases symptoms after dental implantation and eases recovery. Failure to do so from the beginning, aiming for some kind of “clever shortcut,” will hit back at the end of the day.
The second phase of the dental implantation procedure is when the surgical skills of the implantologist shine.
The "second try" is worse than everything
— Dr. Anton Gerasimov
Dental implant placement
Dental implant placement is the easiest step of the whole dental implantation procedure. An implantologist will do local anesthesia (I prefer computer-assisted anesthesia), and you will feel only some pressure and vibrations. The most discomfort could be only because of the cheek retraction or some saline fluid in the mouth. Cheek retraction is necessary for the surgical field overview, and saline is used for irrigation. At the same time, your whole dental implant placement and recovery must be more pleasant than a tooth extraction.
An experienced implantologist will place a single dental implant in approximately 12 to 15 minutes. But a dental chair is not the place for world records.
Guess the most often joke of an anxious patient after a dental implant placement. "I will not treat any tooth anymore. I will replace it with a dental implant once it has a problem. It's the easiest dental procedure." Definitely, the right doctor will never support such a tactic.
— Dr. Anton Gerasimov
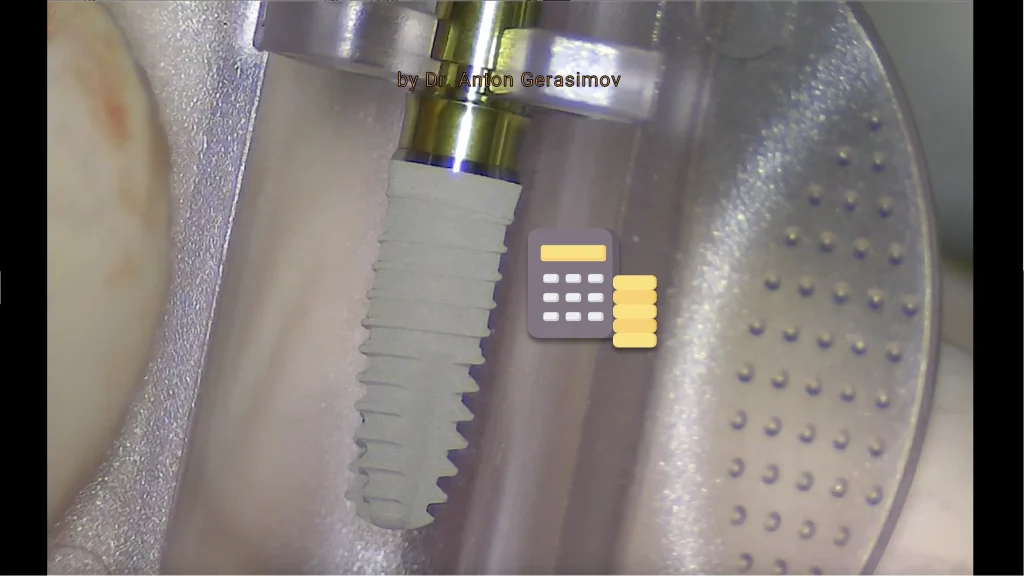
Control of the dental implant placement with mechanical measures
Mechanical control of the placed dental implant is essential for clinical determination of an osseointegration period and other questions. Measures include:
- Dental implant insertion final torque evaluation
- Graph of insertion torque over time analysis
- Dental implant resonance frequency analysis
There is a special equipment for every measure.
Control of the dental implant placement with X-ray
Intraoral periapical digital X-ray is a must at this step. Today it is an irreplaceable diagnostic tool. Additional methods include panoramic radiographs (Orthopantomagram, OPG) and cone-beam computed tomography (CBCT). The former suits the surgery day for a patient with many dental implants inserted simultaneously to do the check faster and return to intraoral X-ray at the next visit. The latter suits challenging and risky clinical cases because it allows 3-dimensional analysis.
The usual mistake is skipping digital X-rays for OPG or CBCT as soon as they seem more beneficial. However, digital X-rays provide the best high-resolution image without any artifacts. Therefore, this early postsurgical digital X-ray is a precious benchmark during the recovery and function of a dental implant for the whole life.
Pharmacological therapy after the dental implant placement
Pharmacological therapy usually consists of antibiotics, pills for correcting intestinal flora, antihistamines, and nonsteroid anti-inflammatory pills. Local treatment typically includes intermittent regional hypothermia and personal oral hygiene. Following the prescriptions the implantologist gave you will increase predictability and decrease symptoms after dental implant placement.
Facultative provisional crown or bridge for the period of osseointegration of the dental implant
Despite common opinion, it is much more predictable to fix provisional prosthetics as soon as possible but not after a week and to load many implants with it but not a single implant temporary crown.
The best time for temporary teeth on implants is 72 hours after a dental implant insertion. Because later, dental implants will lose their primary stability.
The single implant provisional crown is risky compared to a full-mouth dental implant rehabilitation clinical case. The reason is that single-tooth prosthetics will not distribute the load between several implants and is susceptible to non-axial and sheer load to the implant-bone interface. As a result, it can interfere with good healing and bone growth around the dental implant. The result could even be a dental implant failure.
Follow-up after the dental implant placement, suture removal
It is crucial to meet your implantologist on the seventh day.
- All main complaints must be gone until this day
- This visit will verify adequate healing
- It’s time to take out sutures. The influence of prolonged keeping of sutures is slightly negative
- The word of the implantologist always aids
How would you know if everything is more than perfect with a dental implant after a week? The patient mentioned sutures as the complaint.
— Dr. Anton Gerasimov
Osseointegration period (read carefully)
Introduction
If someone breaks a leg, the fractured bone fragments will grow together. Many of you know the secrets – immobilization and time. Immobilization and time are more important than bank accounts in such cases. Even if the top-in-the-world football player breaks a leg, all the best doctors and sponsors’ money will not heal him in a month. Moreover, he will recover much longer than an office worker because a sportsman’s health is super important and his loads are high. White-collar will limp back to the office in 6-12 weeks, and a superstar forward will return after 3-12 months.
Question to you
What do you think if there were a medical possibility for a top-in-the-world athlete to recover in 6 weeks after a fracture for any money or with any doctor? Would he take this possibility at any cost? Would medical manufacturers invest in such technologies if they can?
Explanation
It’s not that the dental implant grows to the bone; your bone grows to it.
Conclusion
That’s all you need to know about the “my dental implants osseointegrate just in one-month” marketing strategy.
For predictability reasons, be ready for at least three months of the waiting period until the final restoration at the lower jaw and four months at the upper jaw (bone is softer). The final osseointegration will end only after up to twelve months of the functional load of the final restoration.
Control of the osseointegration of the dental implant with X-ray
At this stage, intraoral periapical digital X-ray is the golden standard. An implantologist will compare the intraoral periapical digital X-ray with a previous one. Comparison is essential to understand bone behavior during the osseointegration period. Other methods do not provide an acceptable level of precision but may be used occasionally if any suspicions appear or patient-related limitations exist.
Control of the osseointegration of the dental implant with mechanical measures
There could be a mistake at this step. Many implantologists and prosthodontists overuse reverse torque tests after a healing period. As I told earlier in this article, completion of osseointegration depends on subjecting the final restoration to functional load for up to twelve months. Therefore the dental implant is not ready for maximum loading at this stage. Moreover, bone is weakest to shear forces, yet this is the primary force applied with reverse torque testing (Jividen, Misch 2000).
Thus, implantologists can use resonance frequency analysis freely after the healing period and must be very careful and strict with reverse torque testing because early crestal bone loss and dental implant failure may result from this test.
Facultative soft tissue transplantation
Even though soft tissue transplantation can be performed much earlier in the treatment plan in severe clinical cases and later as a step to perfection, it is rational to perform it simultaneously with healing abutment placement on the dental implant. I do not support the fashionable opinion that soft tissue transplantation is inevitable for several reasons:
- Indications for soft tissue transplantation in the exact clinical situation must be formulated. These indications are sometimes unclear at the dental implantation procedure’s start.
- The bone shape will change during treatment, and the soft tissue shape depends on it. Moreover, a clever implantologist will use every surgical intervention during the treatment process to improve soft tissue conditions. Being deficient can become acceptable in the end sometimes.
- While bone grafting is usually ineffective after dental implant placement, soft tissue procedures are.
- In many cases, local soft tissue adaptation will suffice the requirements. But, again, it is the art of using biology in your favor.
- The dental papilla presence after the fixed final restoration relies on fine-tuned prosthetics (Tarnow et al. 1992)
- Substitutes for autologous soft tissue transplants should be considered.
- A lecture could take a long – get a consultation better.
Adaptation of soft tissues around the dental implant
In contrast with the previous paragraph, adapting soft tissues around the dental implant during healing abutment placement is mandatory. Local soft tissue repositioning to get the optimal shape does not influence the patient’s recovery and is very safe to perform after the dental implant osseointegration. Therefore, it’s crucial to focus on developing the local environment for osseointegration during dental implant placement and creating the desired appearance without compromising predictability after achieving osseointegration. Healing abutment placement at this stage dramatically helps because its insertion provides excess soft tissues. Moreover, there is no time for these tissues to degrade because prosthetics will be placed very soon.
Healing abutment placement
Healing abutment – is it difficult?
A healing abutment placement is usually a simple procedure performed under local anesthesia. Usually, it takes about 4-11 minutes for one dental implant.
But in cases of dental implant deep submerging or bone overgrowth during the healing phase, bone profiling is necessary. This objective may be challenging if the dental implant system has no dedicated bone profiler. Actually, most of them have no. If an implantologist does the bone profiling by a free-hand technique, it takes much more time, and a risk of dental implant damage exists. In addition, oversights at this step will result in purulent inflammation 3-5 days after.
One-stage vs. Two-stage protocol of dental implantation procedure
While one-stage dental implants have a transmucosal part and are used with a healing abutment during insertion, more popular submerged dental implants could be used with one-stage or two-stage surgical protocol.
One-stage surgical protocol for a submerged implant means a healing abutment is placed simultaneously with dental implant insertion. Two-stage means that a healing abutment is placed after the dental implant osseointegration.
One-stage dental implantation procedure is better, isn’t it?
Although it’s always tempting to use the one-stage surgical protocol to reduce the number of visits/surgeries for the patient, some disadvantages should be mentioned.
- Actually, the number of visits is the same. After the osseointegration, the dental implant has to be evaluated by the implantologist examination and x-ray.
- The soft tissue adaptation result in the first stage can be lost due to its degradation without prosthetics support. And this loss is almost guaranteed if a patient uses a denture. Therefore the number of surgeries may remain the same. Consequently, second-stage soft tissue transplantation could be indicated. That’s why this approach statistically increases the treatment’s complexity and cost for a patient.
- An oral cavity is not sterile, and its flora may interfere with osseointegration.
- A tongue thrust to the healing abutment provides non-axial loads to the dental implant, which has no positive effect on osseointegration.
- Loosening of a healing abutment sometimes happens during the osseointegration period. An additional visit to the implantologist is indicated to deal with it. Failing to make it fast – and irreversible internal thread damage to the dental implant may occur. Such implants must be replaced with a new one, or continuous crown screw loosening will be forever the curse for this dental implant. Less dangerous but undesirable complications are soft tissue ingrowth under it and wicking of oil-containing food products inside the dental implant. The former must be cut under local anesthesia. The latter must be cleaned appropriately, though it is not easy to have complete control of cleaning.
Conclusion about one-stage and two-stage dental implantation procedure
In conclusion, both approaches have benefits, and an implantologist must consider them wisely.
Hurry up and make people laugh
— Folk wisdom
Facultative adaptation of the provisional prosthetics
If the dental implantation procedure comprehensive plan includes a provisional prosthesis, this step is required. Temporary prosthetics usually are congruent to the shape of the soft tissues. At the same time, a healing abutment is a new structure that prevents the well-fitting of the prosthesis. That is why provisional prosthetics must be modified after a healing abutment placement and soft tissue adaptation. Otherwise, pain and soft tissue recessions may appear.
Control of the healing abutment placement with X-ray
All dental implant systems have their features. Still, no best implant exists. One aspect is the type of implant-abutment connection. Although it is always proprietary for every type of implant, which is a shame, we can divide them into different taper and polygon (typically hexagon) connections. While many dental implant manufacturers promote taper or conical connections, several disadvantages of conical connections exist. One is the absence of tactile feedback for the implantologist during a healing abutment placement. In other words, tight contact at the bone-abutment interface can be taken for the proper contact at the dental implant-abutment interface by tactile feelings of unlucky implantologist. The result could be pain soon after or during the work of an implantologist or prosthodontist, ill-fitting permanent abutments, purulent inflammation after 3-5 days after the procedure, and even early implant failure sometimes.
To be sure that such issues never happen, the healing abutment should be placed perfectly. And besides tactile control, intraoral X-rays must be performed as soon as little doubt arises. Or if the taper or conical connection implant is used.
Soft tissue healing period
The first stage of soft tissue healing around the dental implant and healing abutment finishes in two weeks, but full maturation takes more than five weeks. Luckily, a prosthodontist can typically take impressions or digital scans of dental implants without complete soft tissue maturation.
At the same time, symptoms after the healing abutment placement with soft tissue adaptation should be less intense than symptoms after dental implant placement. Therefore, no pharmacological therapy is needed, and the usual lifestyle is undisturbed.
THE THIRD PHASE OF THE DENTAL IMPLANTATION PROCEDURE
You passed all surgical steps; what can go wrong? If an implantologist just greeted you and inserted a dental implant in the previous phases of the dental implantation procedure – everything can go wrong now. For example, if an implantologist has forgotten to measure the interocclusal distance – a prosthodontist won’t be ever able to place a crown on the implant. Oops.
The leading specialist in this phase is a prosthodontist, not an implantologist. However, after the fixation of the prosthetics, both of them should follow up with you and not forget about you the next day.
But let’s be fair, and patients, too, need to pay more attention to the importance of the proper steps in the third phase of the dental implantation procedure.
A prevalent answer for the follow-up invitation to the clinic is: "All is perfect! I have no complaints, thank you! But, unfortunately, I'm too busy right now for a visit. By the way, my relative urgently needs an implant, and please help him!"
— Dr. Anton Gerasimov
Prosthetics (process, adaptation, correction, provisional, permanent crown or bridge, etc.)
Specialist Prosthodontist performs all the prosthesis works. Before his start, a prosthodontist usually evaluates the actual results of the treatment achieved by an implantologist. To be satisfied before the beginning, a prosthodontist sometimes formulates additional remarks and desires for the implantologist.
It is the standard rule of responsibility distribution between a prosthodontist and an implantologist: if a prosthodontist makes the impressions or intraoral scans – he accepts the results and takes responsibility for the further steps. This borderline is determined because the accuracy of prosthetic work steps determines the outcome of the dental implantation procedure not less than surgical work. However, usually, both specialists act as a team and support the patient in his desires.
This step deserves a separate extended article the same size as this one. But I am only giving you arguments on the subjects of my professional expertise: Oral Surgery and Implantology.
Control of the placement of the prosthetics with X-ray
An ill-fitted abutment, prosthesis, or excessive cement is hard to comprehend without an x-ray. Complications could be acute and early or unexpected and late. To be safe, a prosthodontist will take X-rays after the final prosthesis fixation.
Facultative fabrication of the night guard
Bruxism and clenching are very dangerous parafunctions for the teeth. Not only teeth suffer. Fillings, prostheses, and implants suffer too. They tell you about diabetes and smoking, but bruxism and clenching are significant dangers too. Fortunately, nightguard fabrication and its usage during every single sleep can save your teeth and dental implants. A prosthodontist will refabricate it every 6-12 months, and yes, it’s much cheaper than refabricating your teeth!
A single glance at the night guard in regular use will tell more than a thousand words
— Dr. Anton Gerasimov
Follow-up control of the prosthetics after six months
Although you need to accept the teeth’s type, shape, and color right before the final fixation, two steps earlier; six months of usage are enough for preliminary analysis and final minor adjustments of the whole oral cavity environment for the long functioning of your implants and teeth.
Follow-up control with X-ray of the dental implant after one year
This is an important step. Only now the processes of osseointegration and bone remodeling are complete. The system is working and stable. Previous and new x-rays are essential for comparing and evaluating the current state. If everything is perfect at this visit, the chances of complications and risks are behind.
Annually follow-up and X-ray control of the dental implant and the prosthetics
Your teeth look natural, and you feel comfortable. And now is the most challenging step for you: find a time for the prophylactic examination of the implantologist and the prosthodontist every year because prevention is always better than the treatment, even if the treatment is the dental implantation procedure.
The funniest answer to the follow-up invitation? Well, it was like: "Hi, Dr, I am so glad to hear you, sure I will come, to the same place, right? But you never did surgery on me. I would remember if you did. It was just an examination. What? Implants? Wow! Now I'm remembering something."
— Dr. Anton Gerasimov
- Objectively orchestrate cross-unit.
- Objectively orchestrate cross-unit.
- Objectively orchestrate cross-unit.
- Objectively orchestrate cross-unit.
- Objectively orchestrate cross-unit.
- Objectively orchestrate cross-unit.
Conclusion about dental implantation procedure
As you can see, this page briefly summarizes my almost 20 years of experience in the topic of dental implantation. If you are ready to start a talk about dental implantation, don’t hesitate to contact me directly. Otherwise, you can read about symptoms after dental implantation or check the cost of the dental implantation.